What is Pelvic Girdle Pain?
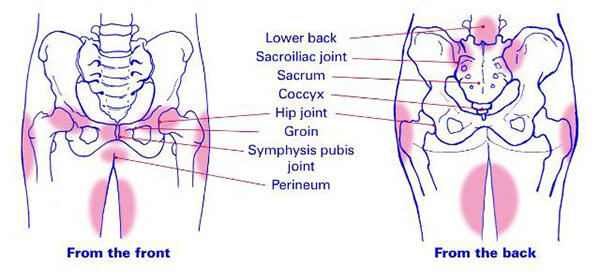
Pregnancy related Pelvic Girdle Pain (PPGP) in the simplest form is pain experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the Sacroiliac joint (SIJ). I know, sounds like a foreign language. The diagram below demonstrates the sites of potential pain as sometimes it can travel slightly into the inner thigh or up into the lower back.
PPGP was formerly known as Symphysis Pubis Dysfunction (SPD). I was very fortunate and didn’t experience PPGP it was something I was prepared for and made modifications when working out if I felt uncomfortable in certain positions. Like we’ve discussed in previous posts, pregnancy wasn’t the time to start hitting those PB’s (for me anyway). I made modifications because I have long femurs and grinding my way out of bottom positions felt rubbish at the best of times! back to the topic title…
So why do some pregnant women experience PPGP? Well PPGP is a common condition affecting 1 in 5 pregnant women (POGP 2018). There are no specifics on when PPGP can start, some studies suggest around week eighteen but it can also develop in the first trimester or as late as three weeks after delivery (Wy et al 2001). Here’s the annoying part, sometimes it’s not obvious why a woman may be suffering with PPGP. There is some evidence to suggest the following may be contributing factors to PGP;
Previous history of low back pain (LBP)
Previous trauma to the pelvis
PGP in earlier pregnancies
Heavy manual work
High BMI
Multiparity (Kanakaris 2010)
Remember the pregnant body is adjusting constantly, structures are being stretched and joints are taking more load. The centre of gravity is constantly shifting to accommodate the growing baby. We become more sensitive around the pelvis during pregnancy this is important as a protective measure. In previous posts we have talked about hormones and the huge role that play in pregnancy and the postpartum period. These hormones have a role to play in assisting the laxity of structures to help the body change throughout the duration of pregnancy. This may sound like I’m describing ligament laxity as if the pelvis may fall apart, it won’t! We need to have a degree of flexibility. There isn’t a large amount of evidence to suggest that these hormones play a role in PPGP. I remember listening to a podcast by Professor Peter O’Sullivan on pelvic girdle pain. He made an excellent point and states there is evidence that ligaments get lax, but there is no evidence that the degree of laxity is a predictor of pain. Prof O’Sullivan interestingly highlights life factors influencing PPGP, lack of sleep, stress, depressed mood, he highlights all of these things as having more of an influence on pain than ligament laxity. And before you say it, lack of sleep… I hear you mama, lack of sleep is life!
What are the functional signs and symptoms of PPGP and how is it diagnosed/ tested? PPGP is partly diagnosed by symptoms described and experienced by the woman during her pregnancy and in the postpartum period. Special tests involving certain movements can also be performed by the GP, midwife or physiotherapist to build more of a picture. Some of the signs and symptoms include;
difficulty walking (waddling gait)
pain on weight bearing through one leg (climbing stairs, dressing)
pain and/or difficulty in straddle movements (getting in and out of bath; turning in bed)
clicking or grinding in pelvic area – may be audible or palpable
limited and painful hip abduction (though some women have normal or only partly)
difficulty lying in some positions e.g. supine, side-lying
pain during normal activities of daily life
pain and difficulty during sexual intercourse
a reduced capacity for standing, walking and sitting
limited abduction (Mens 2006)
What can help with reducing the discomfort? Taking into consideration the things Prof O’Sullivan highlighted around sleep deprivation and mood. It has been clinically proven people who are sleep deprived feel more pain. I know I feel more of everything when I’m sleep deprived. Sometimes my eyes would just sting all day when my daughter was teething and unsettled at night. Trying the best you can to rest and take help when it’s offered is important. If you’re merrily on your way to visit a friend or relative who has recently had a baby, please heed these words. Do not even think of darkening their door unless you are bringing food or intend on holding the baby whilst mama showers/sleeps/eats. Mama and dad do not want to make you a cup of tea or lunch, they will say they do… trust me they don’t mean it they are just being polite. My mum always used to tell me to sleep when baby sleeps and she was so right! It doesn’t matter if the house is a tip or if there’s a mountain of washing up to do, rest is so important and restorative during pregnancy and postpartum.
Limiting moments where you are moving one leg apart from the other (abduction) where possible. I know this is difficult when walking up stairs but limiting this movement where possible will help. Try walking up the stairs one step at a time and leading with the least painful side. Things like getting in and out of the car, in and out of bed. Try keeping the knees together when completing these movements. When getting dressed rather than standing on one leg try sitting down. If you are symptomatic with PPGP reducing time being on one leg may help reduce your symptoms. Trying not to contradict myself in the same breath, staying active to some degree is also important. the supporting muscular structures of the pelvic girdle benefit from movement and exercise in order to stay strong.
Sleeping with a pillow between the knees is important. I didn’t have PPGP but I found myself very uncomfortable at night if I didn’t have my pregnancy pillow which took up A LOT of space in the bed! I’ve put a link to the pillow I used in the references. Having a pillow between the knees helps maintain a form of neutral alignment for the pelvis. Lots of ladies report pain on turning in bed. If possible try squeezing a pillow between your knees when turning, essentially squeezing your bottom muscles.
Make a plan for the day. I know I sound like your mum when I say this but it really does help. A lot of ladies find their PPGP symptoms increase throughout the day so try and get important things done in the morning. Limit trips upstairs by getting things you need downstairs. Move the baby’s changing station downstairs. Use the downstairs loo (if you have one) rather than the upstairs one.
Avoid one sided movements, this includes carrying babies on one hip more than the other and reaching or twisting repeatedly to one side. Have a look at your home or work station and the ergonomic set up. make sure you’re well supported in sitting and not leaning to one side more than the other. If you have an occupational health department at your work place ask to be ergonomically assessed where you sit or spend the most time. Try your best not to cross your legs. This is a good thing to remember anyway and may potentially help baby get into a nice head down position.
These are all useful tips to help reduce symptoms of PPGP. Unfortunately these may only go so far to reducing symptoms and I would urge any ladies who experience persistent symptoms to either discuss a referral to a physiotherapist. Please don’t wait for your next midwife appointment if you are in pain, contact your GP to be assessed and referred to a physiotherapist. Once assessed by a physiotherapist these are the following things we will be looking to improve or advise on (as well as what has been discussed above). You may get slightly fed up with being asked if you’re sleeping with a pillow between your knees!
Things your physiotherapist will look at include your general strength and ability to perform functional tasks. Lots of little tests looking at how your body moves and acts against resistance give your therapist a better idea of what structures may be weak or need a bit of support to reduce your symptoms. Treatments my include exercises to maintain or build strength in the pelvic floor, pelvic girdle, spine and hip region. Motor control rehabilitation and specific limbo-pelvic stabilisation can be helpful (hello modified pilates). In actual fact EU guidelines (2008) recommend specific stabilising exercises including local and global muscle systems as a treatment for PPGP. It may be appropriate to carry out manual therapies like mobilisations and or manipulations, stretches and muscle energy techniques. Physiotherapists can also give advice around pain control and the use of TENS or acupuncture. Finally a physiotherapist can advise on the use of physical support, this may be in the form of a pelvic girdle support belt or something as simple as tubigrip. Sometimes if symptoms persist and worsen increasing support is needed in the form of elbow crutches or the use of a wheelchair. Please don’t let that worry you! I know as soon as things like wheelchairs and crutches get mentioned the tendency is to worry. There are lots of modalities of treatment as mentioned above that your physiotherapist can exhaust in the first instance.
Vleeming et al 2008 describe approximately 20–25% of all pregnant women suffering from PGP that is sufficiently serious to require medical help. The European guidelines for the diagnosis and treatment of PPGP recommend individualised exercises in pregnancy, an adequate supply of information about the condition, and reassurance for patients as part of a multifactorial treatment focusing on specific exercises for motor control and stability postpartum. Although the evidence is scarce on PPGP Morkved et al (2007) completed a random control trial with 301 healthy pregnant women. The study had exercise programmes including pelvic floor muscle training, local and global muscle strengthening with an aerobic and stretching component. They found at 36/40 weeks gestation and 3/12 weeks postpartum the group who were given the exercises showed significantly lower incidence in PPGP than the control group. In a study conducted by Stuge et al (2004) 20 weeks of specific stabilising exercises (like modified pilates) was found to be superior to non individualised physiotherapy in postpartum PPGP. Improvements were seen in quality of life and physical ability with a reduction in pain.
PPGP is probably one of the topics I get most frequently asked questions about. Expectant mothers and ladies already with babies are busy! Lifting things moving bending and twisting is a part of everyday life. Often ladies are working right through to the later weeks of pregnancy. I managed to get to 38 weeks and 4 days, my manager constantly looked worried I was going to have my baby at work! Your physiotherapist will want you to continue your normal fitness routines and functional activities of daily living. They will work with you to achieve goals specific to you. If you are experiencing discomfort during pregnancy or postpartum speak to your midwife or GP about being referred to either a specialist MSK physiotherapist or a women’s health/ pelvic health physiotherapist. Please remember if you have had your baby you should not be in pain, pelvic girdle pain can persist and sometimes even start during the postpartum period for all of the reasons listed several paragraphs above.I hope this little round up on PPGP has been helpful. Remember how important you are as an expectant mother, new mum or mother of 3 or 13. Healthy happy mum, healthy happy baby. Your quality of life and ability to move pain free are important, you are important! Big love V x
References
Kanakaris N. K., Roberts C. S. & Giannoudis P. V. (2011) Pregnancy-related pelvic girdle pain: an update. BMC Medicine 9: 15. DOI: 10.1186/1741-7015-9-15.
European guidelines on the diagnosis and treatment of pelvic girdle pain VL - 17 DO - 10.1007/s00586-008-0602-4 JO - European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society.
Mens JM, Damen L, Snijders CJ, Stam HJ. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomech (Bristol , Avon) 2006; 21(2):122-127.
Mørkved S, Kjell Åsmund Salvesen, Berit Schei, Stian Lydersen & Kari Bø (2007) Does group training during pregnancy prevent lumbopelvic pain? A randomized clinical trial, Acta Obstetricia et Gynecologica Scandinavica, 86:3, 276-282, DOI: 10.1080/00016340601089651
Stuge A, Britt, MSc, PT*; Lærum, Even, PhD†; Kirkesola, Gitle, PT‡; Vøllestad, Nina, PhD* The Efficacy of a Treatment Program Focusing on Specific Stabilizing Exercises for Pelvic Girdle Pain After Pregnancy: A Randomized Controlled Trial, Spine: February 15, 2004 - Volume 29 - Issue 4 - p 351-359 doi: 10.1097/01.BRS.0000090827.16926.1D
Vleeming A., Albert H. B., Östgaard H. C., Sturesson B. & Stuge B. (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal 17 (6), 794–819.
Wu W. H., Meijer O. G., Uegaki K., et al. (2004). Pregnancy-related pelvic girdle pain (PPP), 1: Terminol- ogy, clinical presentation, and prevalence. European Spine Journal 13 (7), 575–589.
My pregnancy pillow was by Theraline and can be found here; https://www.amazon.co.uk/Theraline-Perfect-Pillow-Pregnancy-Nursing/dp/B0764GG6SK/ref=sr_1_5?